Categoría: Bipolar Disorder
Etiquetas: #getba, #mental health, #psychiatry, #treatment
More content you may find interesting
Last Friday, May 18th, I had the opportunity to attend an educational event titled “Bipolar updates, 2018,” which was held in the city of Málaga. The event was led by Dr. Pedro Iborra, a psychiatrist at the San Juan de Alicante day hospital, where he primarily treats patients with borderline personality disorder. Additionally, Dr. Luis Gutiérrez Rojas, whom I am pleased to know, as he is the president of GETBA, a scientific association in Andalusia focused on bipolar disorder, of which I am a member. Dr. Gutiérrez Rojas will likely supervise my thesis in the not-so-distant future.
During these talks, three specific topics were addressed:
The first topic discussed was the concept of “empowerment” of the patient, which essentially involves empowering and strengthening the patient and their family so that they can actively participate in self-care. This entails not only informing the patient about their condition in plain language but also educating and training them regarding their health, enabling them to gain awareness and competence about their illness. This, in turn, facilitates empowerment, self-management, self-confidence, and ultimately leads to greater treatment adherence and positive changes.
In essence, it involves the patient actively facing their illness, becoming involved in managing their own health. In this way, the patient becomes well-informed about their condition and the best ways to address it, promoting responsible use of resources (for example, knowing when to urgently seek medical help based on signs or symptoms).
Not so long ago, the role of the doctor was paternalistic, where the patient placed themselves blindly in the hands of their doctor, and the doctor made decisions they deemed best for the patient. Nowadays, the role of the doctor has changed, and what we should do is inform the patient in language adapted to their level of understanding so that the patient can freely make decisions about different treatment options, weighing the pros and cons. This encourages teamwork between the patient and therapists to promote the patient’s well-being together.
The second topic discussed was “translational psychiatry,” which, to avoid excessive elaboration, involves translating the various research findings into clinical practice. Often, genes implicated in diseases or brain imaging findings that are more common in people with a mental illness than in healthy individuals are discovered, to name a few examples. But what practical application do these findings have? It’s not always easy to find such utility because mental illnesses are complex, multifactorial, and difficult to objectify or measure. Translational psychiatry seeks to bridge the gap between theory and practice.
The final topic discussed on this productive day was the molecule asenapine (brand name: Sycrest or Saphris in other countries). It is an atypical antipsychotic approved by the FDA for acute and maintenance schizophrenia (in the United States) and for the manic or mixed phases of bipolar disorder (in the United States and Europe), either as monotherapy or in combination with a mood stabilizer like lithium or valproate. It is also used for the maintenance phases of bipolar disorder.
This was quite an interesting discussion as all the attendees and speakers were able to share their experiences with the use of this drug in clinical practice.
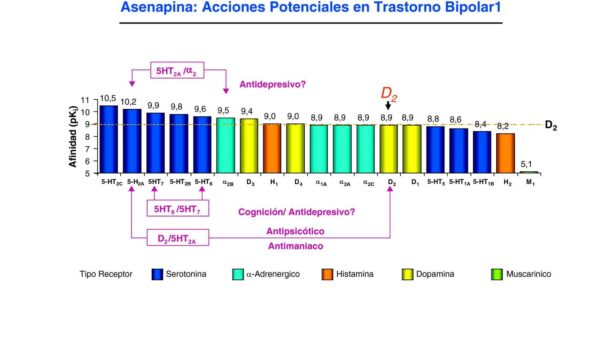
The image above shows all the receptors that asenapine interacts with and its affinity for each receptor. Thanks to its receptor profile, pharmacokinetic, and pharmacodynamic characteristics, asenapine can offer some advantages over other antipsychotic medications.
For those who aren’t experts in the field, it’s worth noting that one of the standout features of this molecule is its rapid action compared to other antipsychotics because it’s administered sublingually (under the tongue). This not only allows for shorter hospital stays but also bypasses the liver, which is especially useful for patients with hepatitis or fatty liver conditions. Asenapine also has potential anxiolytic effects without being overly sedative, which means it calms without the need for benzodiazepines (anxiolytics like clonazepam, alprazolam, diazepam, etc., which are useful for anxiety but can be addictive). Overall, it is well-tolerated.
One of the main drawbacks? Its famously bitter taste, and you shouldn’t eat or drink anything for at least 10 minutes after taking it to avoid altering its absorption. As mentioned, it’s sublingual, meaning you place it under your tongue and wait for it to be absorbed within a few seconds. It should not be chewed or swallowed because if it’s swallowed, it won’t have any effect. Some patients use a little trick to make it less unpleasant by using mouthwash (e.g., Listerine) before taking it. The mouthwash numbs the mouth slightly, making the experience less unpleasant.
That’s all for today. I’ll leave you with a couple of images from Málaga. Until next time!