Categoría: Psychotic Disorders
Etiquetas: #schizophrenia, #studies, #technology
More content you may find interesting
This past weekend, I had the opportunity to attend an excellent lecture by Dr. Julio Sanjuan, a Psychiatry professor at the University of Valencia and coordinator of the First Psychotic Episode Unit at the Valencia Hospital. The lecture took place in Málaga as part of the 10th Update Course in Psychiatry organized by the Castilla del Pino Foundation. For those who may not be familiar with him, Dr. Sanjuan, in addition to being a psychiatrist and a professor, also dedicates time to research. During his presentation, he decided to share one of his most recent findings, which I will also discuss in the latter part of this text.
Before delving into that, as Dr. Sanjuan did in his lecture, let me provide some context for the readers:
In 1992, the first scientific publications appeared, supporting the idea that early treatment in psychotic episodes leads to a better prognosis. Concepts like “untreated psychosis duration” (the time that elapses between the onset of the first psychotic episode and the initiation of treatment) and “untreated illness duration” (which includes the aforementioned and the “prodromes”) gradually became more widely known.
“Prodromes” are nonspecific symptoms that precede a psychotic episode and may indicate which individuals are at risk of experiencing a first psychotic episode, sooner or later. Examples of prodromes include social withdrawal, mistrust, loss of motivation or interest, or impaired functioning (academic failure, job loss, etc.). These symptoms are highly nonspecific, as they can also be present in other situations, and having them doesn’t necessarily mean one will experience a first episode. However, they should raise awareness of this possibility, especially in certain population groups.
Therefore, the first early intervention programs were created with the idea of detecting individuals suffering from psychosis as early as possible, initiating treatment promptly, and improving their prognosis and outcomes.
In 2005, J. Bertolote and P. McGorry, with a substantial budget, established an early intervention program and published a consensus statement in the British Journal of Psychiatry titled “Early intervention and recovery for young people with early psychosis: consensus statement.” In summary, they emphasized five key points that should be addressed:
Early detection in the community.
Early detection in primary care.
Facilitating rapid access to treatment for patients.
Promoting the recovery of everyday life in patients.
Involving and providing support to the families of these patients.
In addition to their importance and utility, first psychotic episode programs have proven to be cost-effective, meaning they save the government money. This may explain why there are about 150 such programs in the UK. However, what about Spain?
In Spain, only the Balearic Islands and Cantabria have programs that cover the entire population, and in Catalonia and especially Navarra, these programs have received specific funding. In the rest of the country, there are either very few or no programs, and if they exist, they lack dedicated funding. Furthermore, there is no consensus regarding the formation of these programs, whether in terms of their duration (which can vary from 3 to 5 years), the target population (early vs. all ages), or the involvement and coordination of various healthcare facilities with the program. Therefore, it seems essential to come together to unify criteria and conduct further research to determine the critical variables when creating such a program.
Ideally, according to Dr. Sanjuan’s program, and recognizing that this might sound utopian in clinical practice, clinical assessment tools should include:
- The PANSS scale (which assesses positive and negative symptoms in the subject).
- Collection of risk factors (substance use, childhood abuse, immigrant status, degree of insight, or premorbid adjustment).
- Functionality scales: PAS, SFS…
- Neuropsychological assessments: conducting a SCIP as a screening tool, and if it shows pathology, proceeding to an MCCB (MATRICS Consensus Cognitive Battery), which is a cognitive assessment battery.
- Estimation of the Intelligence Quotient (WAIS vocabulary).
- Adherence scale.
- Performance variation scale for both family members and patients (SCoRS).
- Brain imaging: Magnetic Resonance Imaging (MRI) is preferred over CT scans because MRI provides more information and white matter resolution. When psychotic symptoms appear, between 3-8% of cases show specific neurological findings (brain tumors, stroke, multiple sclerosis, etc.), so excluding these possibilities as part of the initial screening for a first psychotic episode, in addition to a blood test and a thorough neurological examination, is essential.
Today, through functional magnetic resonance imaging (fMRI), it is known that many brain areas become hyperactive during a first psychotic episode. In the image below, you can see an example of how functional magnetic resonance imaging is done in patients with schizophrenia.
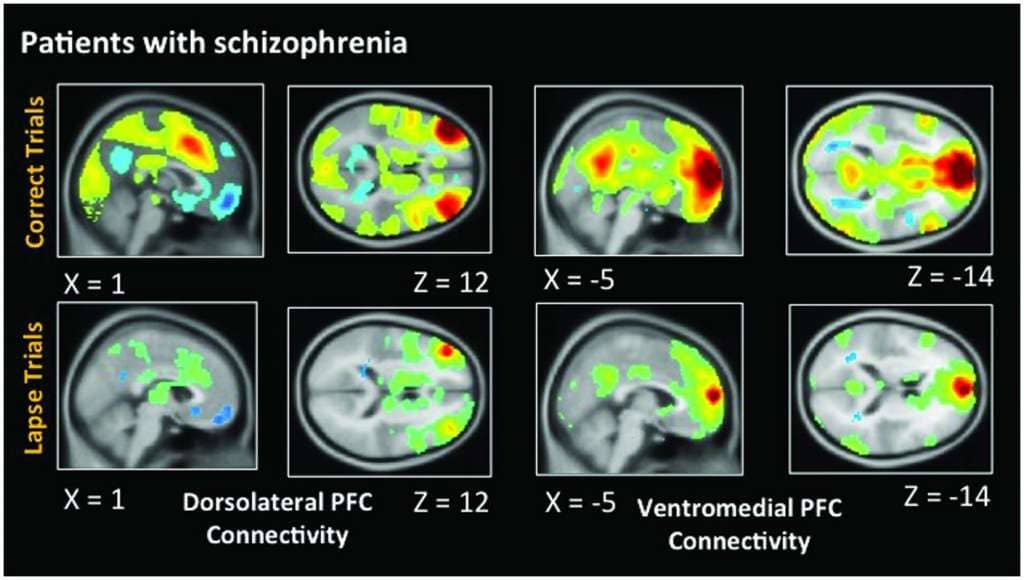
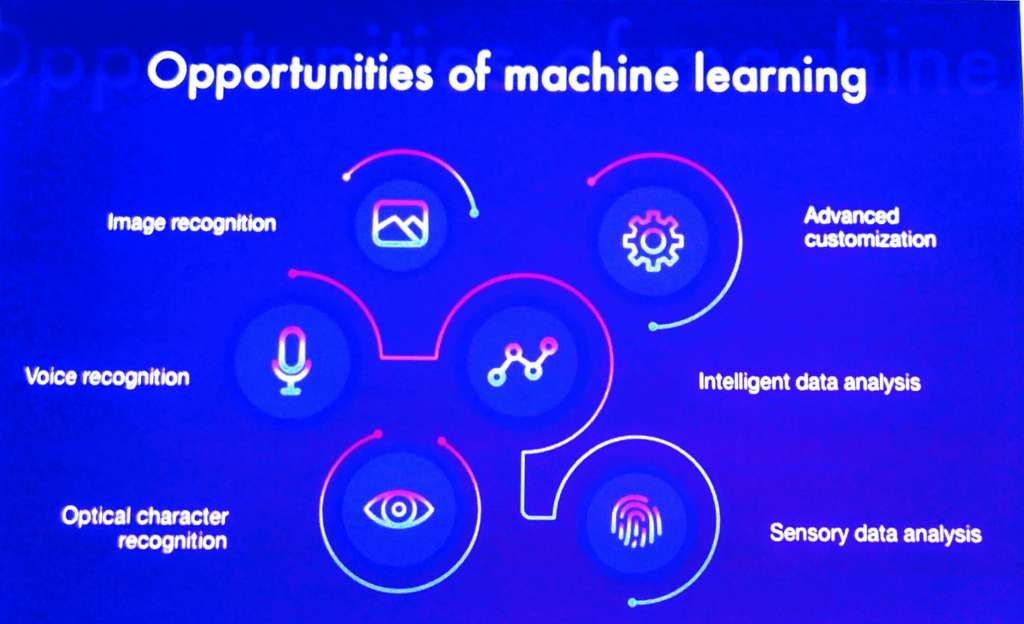
On the other hand, there’s something known as “machine learning,” a subfield of Artificial Intelligence that combines neuroscience and computer science. In very simple terms, machine learning involves computers analyzing millions of data points to identify patterns and learn from them to predict outcomes. While this has many applications, in the context we’re discussing today, there are a total of 64 published studies that combine neuroimaging techniques (fMRI) with machine learning in schizophrenia. The goal is to determine if using machine learning to analyze data can accurately diagnose schizophrenia. However, to date, the results have been somewhat discouraging, as these studies have only achieved a diagnostic accuracy of around 60%…
…Until today! Here comes Dr. Sanjuan’s exclusive revelation: in a recent study he conducted, with results obtained in late 2017, and not yet published, they achieved an overall accuracy of 90%!
How did they do it? They used functional magnetic resonance imaging data (with an emotional auditory paradigm, which might be key) in combination with those machine learning techniques. This is the first time such results have been achieved, and if the findings hold true, it would be a significant breakthrough in psychiatry because it implies they might have found biological markers for schizophrenia.
That’s it for today’s post. I apologize if it was a bit technical and less informative in this case, but I couldn’t resist sharing these findings with you. We eagerly await the publication of Dr. Sanjuan’s results. Be sure to check out his publications on PubMed for more information.
Happy Sunday!