Categoría: Overweight and obesity
Etiquetas: #bariatric, #obesity, #overweight, #psychiatry, #surgery, #weight loss
More content you may find interesting
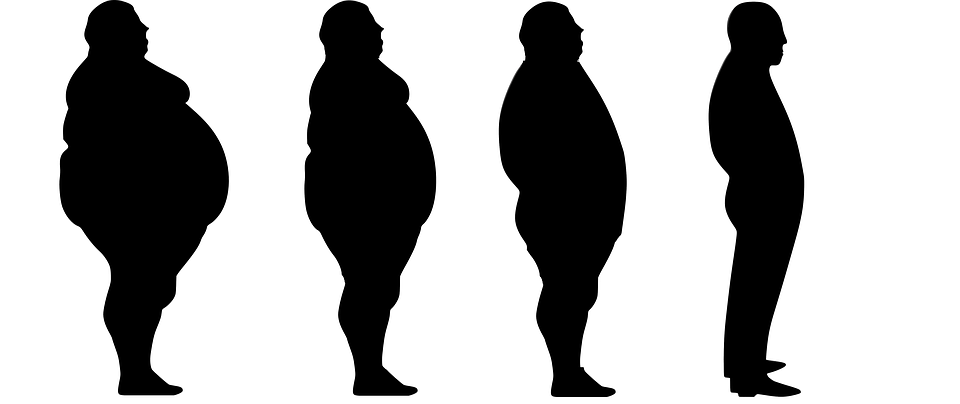
Obesity is a significant public health problem. When we talk about morbid obesity, we are referring to a high-risk chronic condition defined by a Body Mass Index (BMI) of 40 or higher. Morbid obesity carries negative health consequences for both physical and mental health.
Obesity is associated with reduced economic, employment, and social opportunities, decreased quality of life, and is a determinant of various risk factors leading to increased mortality and a decreased life expectancy (Ricci MA et al., 2016).
Both depression and obesity are highly prevalent and represent some of the most significant public health issues today (Jantaratnotai N et al., 2017). Obesity is not only associated with depression but also with a higher prevalence of other mental disorders (eating disorders, anxiety disorders, etc.).
With the increasing prevalence of morbid obesity in recent years, there has also been an increased demand for bariatric surgery. This procedure results in improvements in metabolic disorders, cardiovascular risk, and patient mortality (Ricci MA et al., 2016). However, not everyone is a candidate for this surgery.
Given this, what role does a psychiatrist play in the treatment of morbid obesity? Their primary (but not exclusive) roles include:
- Assessing the patient’s capacity to make an informed decision regarding surgical treatment. This involves evaluating whether the patient comprehends the implications of the surgery, can weigh its consequences, and is capable of making a free decision about whether to proceed with the surgery or not.
- Detecting potential mental disorders and psychopathology in surgical candidates, with the goal of treating these conditions if they exist. This can eliminate potential exclusion criteria for surgery, contraindications, or situations that may hinder proper adherence to the treatment plan, which could compromise the success of the surgery.
- Determining the need for psychotropic medications to help maintain the necessary behaviors for weight reduction (e.g., anxiolytics, antidepressants, or others as needed).
In broad terms, according to Ríos (2010), psychological contraindications for bariatric surgery can be categorized as follows:
Absolute Contraindications:
- Adjustment disorder following a recent experience
- Decompensated psychiatric disorder (psychotic episode, manic or depressive phase in bipolar disorder, active purging bulimia, active binge-eating disorder, recent suicide attempt)
- General risk situations: alcohol or drug abuse, profound mental retardation
- Limited support from the social or family environment
- Low motivation on the part of the patient to undergo surgery (e.g., patients pressured by their partners or family)
Relative Contraindications:
- Previous history of bulimia (at least one year of remission is recommended)
- Previous history of alcohol or drug abuse
- Identification of secondary gain related to obesity
- Considering surgery as a solution to difficulties related to their work, social, or family environment
- Dysfunctional family environment
- Unresolved grief, recent divorces, previous suicide attempts
If you wish to make an appointment for a preoperative psychiatric evaluation, please do not hesitate to contact info@doctorapaulamoreno.com or call +34688996798, and we will assist you as soon as possible.





